Have you ever been told that you have “sciatica”? Or have you consulted Dr. Google about buttock or leg pain and self-diagnosed it as “sciatica”? The term is a popular one and has become a blanket term for nerve-related issues that affect the lower extremity.
What is sciatica?
The classic symptoms of sciatica are sharp, electric shock type of pain that radiates down the back of the thigh into the lower leg, sometimes accompanied by numbness or tingling.
One of the reasons the sciatic nerve gets a lot of press is due to its unique nature anatomically in the body. The sciatic nerve is the largest nerve in the body, about the width of a pencil, and originates from nerve roots in the lower lumbar spine and sacrum. It branches out of the lumbosacral plexus, a bundle of nerves in the pelvis, travels into the buttock region and down the back of the thigh. As it courses through the gluteal region, the sciatic nerve runs either beside or directly through the piriformis, a deep buttock muscle (anatomy differs slightly from person to person).
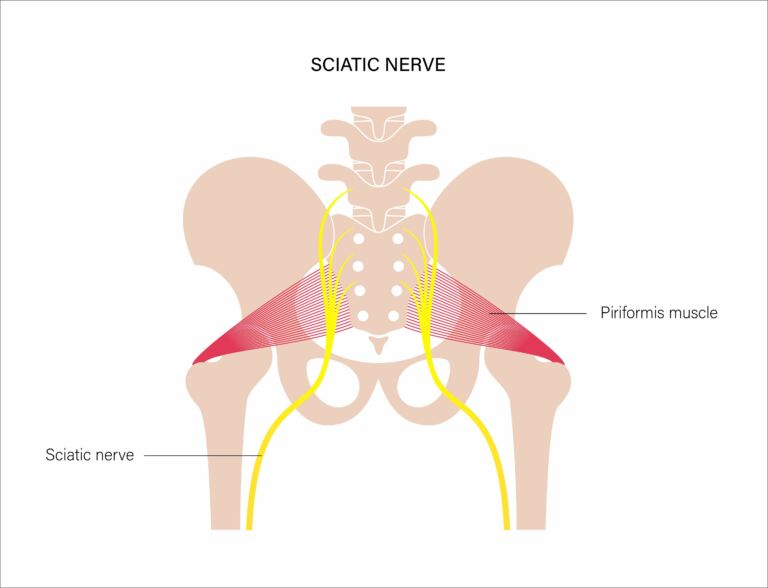
In theory, a tight piriformis muscle can be a source of irritation of the sciatic nerve, creating compression around the nerve that generates sharp pain and sometimes numbness/tingling radiating down the leg.
After coursing through the hip and thigh area, the sciatic nerve divides further into the tibial nerve and the common peroneal nerve near the knee area, which supply the lower leg with strength and sensation.
What causes sciatica nerve pain?
Sometimes, sharp pain radiating down the back of the leg is truly related to the sciatic nerve being irritated in the hip or buttock region, and we may call this “piriformis syndrome.”
Stretching and releasing the piriformis muscle with soft tissue techniques can help provide relief. But it’s important to consider that a more common source of radiating leg pain (along with numbness and/or tingling) is what we refer to as nerve root irritation from the lumbar or sacral regions. In these cases, the sciatic nerve has become irritated further up the chain – closer to the vertebral column where the nerves L4, L5, S1 and S2 branch out from the spinal cord between the vertebrae.
If the source of the leg pain is the spine vs the hip, treatment may look quite different!
How is sciatica diagnosed?
Physical therapists are the optimal choice to identify the source of pain in the lower back or buttocks that radiates or shoots down the leg.
During a physical therapy exam for “sciatica,” your PT will take time to learn a thorough history, including finding out what positions increase pain and what positions relieve it. Additionally, your physical therapist will work to understand how your pain is affecting your daily life – this is an important part of the evaluation.
The physical exam will include sensation, reflex and strength tests throughout the lower leg to assess nerve-related function, as well as flexibility tests to determine how sensitive your nerves and muscles are to stretching.

Testing of the sacroiliac joint may also be performed (especially in women during pregnancy or postpartum who are experiencing buttock pain). The differential diagnosis process is key because it directs the treatment approach. A misdiagnosis and focus on stretching and massaging your piriformis muscle to relieve sciatic pain may not give you long-term relief if the radiating pain is related to your lumbar spine or sacroiliac joint rather than generated from the buttock region.
How is sciatica treated?
Once your physical therapist has diagnosed your sciatica nerve pain, they will work with you to establish functional goals and create a custom treatment plan to address your symptoms. Your plan of care can help reduce inflammation and pain, improve your physical function, treat the underlying cause of your sciatica nerve pain and prevent future flare-ups.

If the source of the symptoms seems to be the lumbosacral spine, physical therapy may include manual therapy like joint mobilization or traction applied to the stiff or irritated spinal segments. If the symptoms are related to tight/overactive gluteal muscles, soft tissue mobilization (massage) may be used to release muscle tension.
Exercise prescription will also be key – there may be stretches that can give you immediate relief, whereas strengthening the muscles in your core may provide long-term relief.
Usually, physical therapy for sciatica will include 8-12 visits over the course of 4-6 weeks to get you to where you can independently manage any remaining symptoms and have met most, if not all, of your goals.
How can I test myself for sciatica?
If you suspect your pain is sciatica, a self-test you can do at home is to check your tolerance to repeated flexion and repeated extension.
Standing up, bend forward and reach down toward your toes. Come back up and then bend forward again for a few repetitions. If you feel the pain reproduced and radiating down your leg, this is called peripheralization.
Now, try bending backward with your hands on your hips. Come back up and then bend backward again. Go through a few repetitions. If the pain moves out of your leg and into your back, this is called centralization.
If repeated flexion causes peripheralization of your symptoms and repeated extension causes centralization of your symptoms, this indicates that you may have a nerve root irritation coming from the spine.
If you don’t have any change in your leg symptoms with forward or backward bending, you may have a true sciatic nerve irritation in the hip.
One way to help determine this is to try sitting in a “figure 4” position, with the affected leg crossing over the opposite leg (ankle over the opposite knee). If this reproduces your leg symptoms, you may have sciatica that is related to tension in your piriformis and other deep buttock muscles.

Does sciatica go away on its own?
If you’re experiencing peripheralization or centralization, consistent with nerve root irritation from the lumbosacral spine, you may respond best to exercises such as the prone press-up (cobra) along with core stabilization exercises including bird dogs, planks and bridges.




You may also consider using a lumbar roll or a rolled-up towel with rubber bands or tape around it to keep your back slightly arched when sitting for long periods of time such as while working at a computer or while driving.
These strategies aim to reduce irritation around the nerve roots from the lumbosacral spine. By focusing on extending your spine frequently, you can essentially pump the inflammation away from the nerve root and relieve the pressure on the nerve (if the pain is moving out of your leg and into your low back, that is a sign you are doing the right self-treatment!). The core strengthening exercises help to prevent the irritation from returning.
When should I see a physical therapist for sciatica?
If your sciatica symptoms last for more than a week or two, are spreading further down your leg or into both legs, or you are experiencing new symptoms like numbness or tingling, reach out to a physical therapist to get in for an evaluation. These are signs that the nerve irritation may not be going away on its own!
Research shows that getting in for physical therapy within 14 days can significantly improve your chance of a great outcome.
Many of our patients with sciatica describe difficulty with sitting, driving, walking and sleeping – if you are having trouble with daily functions like these, you should not keep living with these difficulties. In your first 3 visits with a physical therapist, you are likely to experience some improvement and relief of your symptoms, with a plan to get you back to 100% function within a few weeks.

Start your physical therapy journey today.
As physical therapists, we know the importance of movement for overall health and well-being. From injury recovery to achieving optimal performance, our passion is to help every patient reach their goals and live an active, pain-free life. Get started with PT today!

