The Temporomandibular Complex (TMC)
The Temporomandibular Complex (TMC) is the medical term for your jaw, the jaw joint, and the surrounding muscles that control chewing and jaw movement. This complex includes the muscles of mastication (chewing) and the Temporomandibular Joint (TMJ), which includes tendons and ligaments of the jaw.
You can find your own TMJ by feeling the boney bump just in front of your ears that moves as you open and close your mouth. This joint is flexible and allows the jaw to move up and down and side to side, affording us the ability to eat, laugh, talk, yawn, and even sing.
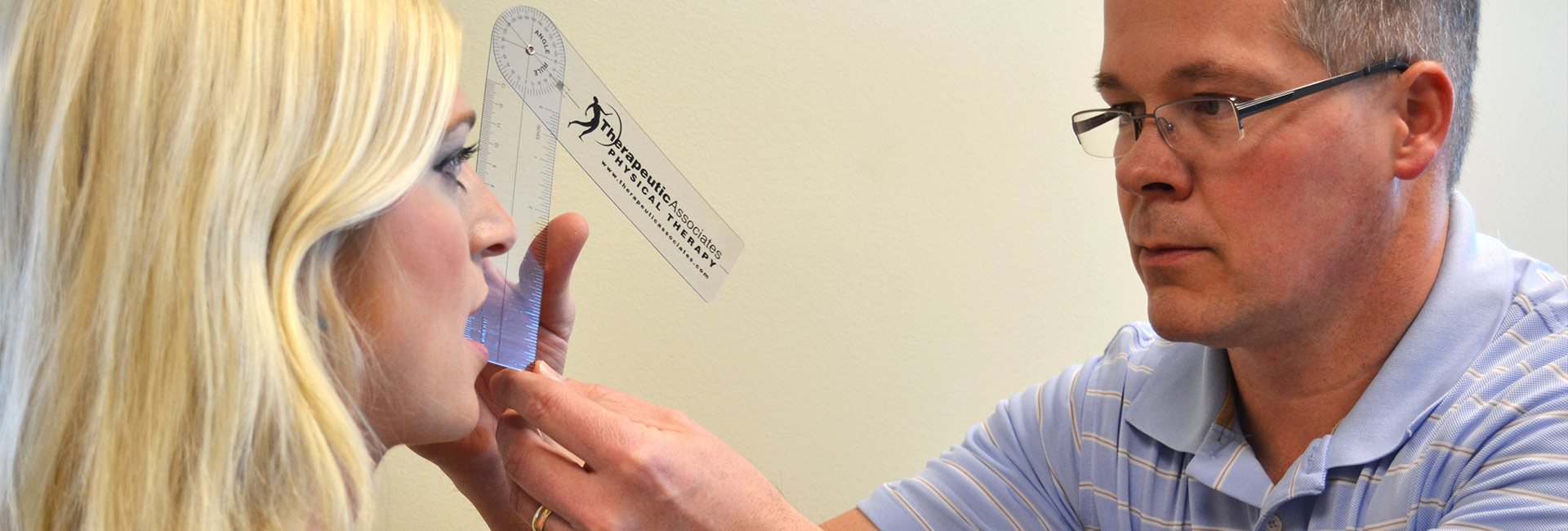
Temporomandibular Disorders (TMD) can include a variety of conditions that cause tenderness and pain in the TMJ and surrounding areas. Most recent research shows that TMD’s can be contributing factors to neck (cervical) pain, dysfunction, and injuries.
As the awareness of TMD increases, it is important to discern the various sources of facial pain.
Several muscles other than the muscles of mastication (chewing) can cause pain to the TMC area. Examples of this include the sternocleidomastoid (SCM), a neck muscle often injured in car accidents, which can refer pain to the chewing muscles and can cause ringing in the ears and dizziness. In addition, an imbalance in the upper trapezius muscle of the neck caused by sitting without arm support or by constantly elevating the shoulders can present as a disorder of the TMC.
There is also a strong clinical correlation between dysfunction of the cervical spine, particularly the upper portion, and involvement of the TMC. This onset may be secondary to trauma, such as a fall or a motor vehicle accident, or it may be related to chronically held tension or poor posture.
Posture and Biomechanics
IDEAL POSTURE occurs when your head is balanced over your shoulders with your chin parallel with the floor and the shoulders relaxed. When the center of gravity of the head is balanced over the neck properly, there is a physiological state of rest in the head, neck, and shoulder muscles. In ideal head posture the head is almost wholly balanced upon the cervical spinal column.
FORWARD HEAD POSTURE is the most common poor postural alignment. Some believe that as a reaction to forward head posture, the muscles used for chewing are overworked to keep the mouth closed. A review of the literature demonstrates that forward head posture has a significant influence on Electromyographic (EMG) activity of the chewing muscles and joints when at rest. There are also correlations with head posture and craniofacial pain patterns.
Patient Awareness
Before patients can be expected to correct their posture, they must be made aware of what ideal posture is and how it is different from their current use of their body. In addition to this education, patients must also develop a sense of what the ideal head and neck position feels like. This is accomplished through various postural exercises individualized to each patient’s needs and includes instruction in the normal rest position of the tongue.
The normal rest position of the tongue is with the tip of the tongue resting against the roof of the mouth, just behind the front teeth. This is a soft rest position, as if you were saying “N” very gently. If you are not chewing or talking, this is the position where your tongue should be resting to promote the most relaxed position of the TMC.

Achieving a Balanced System
Tight muscles must be relaxed and returned to their normal length. Overstretched muscles must be strengthened. Any restriction in joint mobility (cervical, thoracic, scapular, or temporomandibular) must be restored. Manual therapy techniques, including soft tissue mobilization, joint manipulation, and specific stretching methods are often necessary to initiate the restoration of normal posture. Life-style changes often need to be made with the implementation of techniques for coping with stress, promoting relaxation, and eliminating counterproductive postural habits. Poor postures and emotional stress are the most common perpetuating factors of head and neck pain and dysfunction.
Changing Old Habits
Forward head posture is a learned behavior, and in order to replace this old habit with a new position, it requires frequent repositioning and positive input to the musculoskeletal system. Patients are asked to do their exercises every hour and must consistently follow through on a daily basis for a 30-day time period. Patient compliance is essential for a full recovery.
Evaluation of the Occupational Environment
In addition to establishing the feel of ideal posture and actively making changes to balance the musculoskeletal system, patients must be shown the correct posture for various activities for daily living.
For example, if a patient stands for the majority of the day, he/she is taught to shift the weight to the center, or toward the ball of the feet, and to equally distribute the weight between the right and the left foot. This position moves the forward head back over the shoulders and reestablishes the ideal center of gravity. For the office worker who is required to sit all day, correct use of a good chair is required to support the upper body. The correct height of the work surface, chair, computer, etc. must also be addressed. If any of these areas are at the wrong height for a particular individual, they become an aggravating factor that can trigger myofascial pain symptoms.
Myofascial pain can be a major problem for those with neck and Temporomandibular dysfunction. However, with the correct guidance, perpetuating factors can be eliminated, old habits can be changed, and a balanced postural system can be attained.
Are you experiencing myofascial pain?
Our specialists are committed to the application of evidence-based treatment techniques to ensure you experience the best in rehabilitation and preventative care and see progress with every visit.