Of all the back injuries we see as physical therapists, there may be no greater misunderstood injury than the herniated disc. Most everyone has heard the terms “herniated disc,” “bulging disc,” or “slipped disc,” so, when someone experiences low back pain this injury often comes to mind as a potential explanation. Some questions we as physical therapists often encounter surrounding disc injuries include:
- Do I have a herniated disc?
- Will I need surgery if I have a herniated disc?
- Can physical therapy help correct a herniated disc?
There’s a lot of information to unpack regarding what a herniated disc is, how to know if you have one, and if so, how physical therapy can aid in healing and recovery.
Let’s dive into it.
What is a spinal disc?
Situated between each bony vertebra in our spine is an intervertebral disc. These discs play a pivotal role in allowing for movement between the vertebra while also being a shock absorber and accepting the different stresses our back and neck experience during daily life.1 So, for example, if you were to bend down to pick up a laundry basket off the floor or were enjoying a more repetitive activity such as hiking, these discs help absorb the shock and minimize stress on your back. As we age our discs naturally experience wear and tear and become smaller, which is part of why as we age our bodies are not as good at tolerating this type of stress.
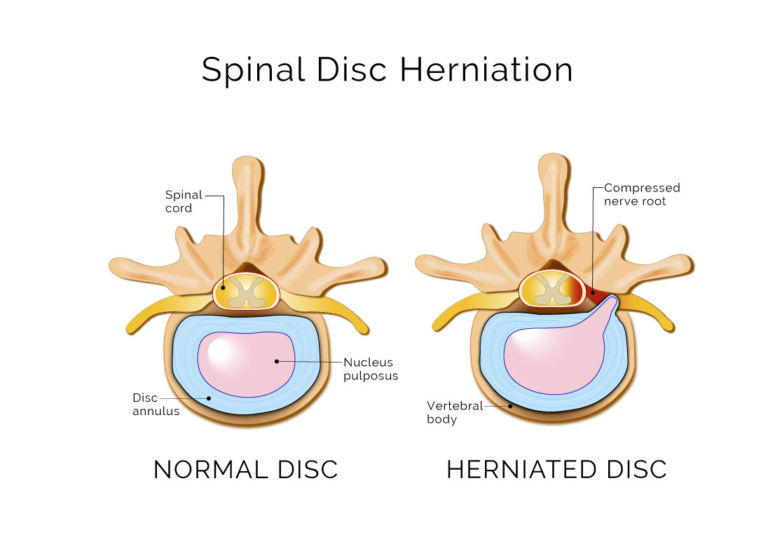
The disc is composed of a tough outer layer (annulus) and an inner component (nucleus pulposus, or NP) which is roughly 80 percent water and has a consistency similar to toothpaste.2
As we age, our discs experience natural wear and tear and ultimately lose some of their height.3 Studies estimate that half of individuals 60-69 years old have moderate-to-severe disc space narrowing (DSN).4 The effects of aging on spinal discs can be detected even earlier, however. For example, a 2012 study by Goode et al. looked at x-ray imaging findings of DSN in a healthy population of those 45 and older. Of the 840 participants, more than half (57.6 percent) showed some level of DSN. 3
What is a herniated disc?
Is a herniated disc always painful?
Having a herniated or bulging disc does not necessarily mean you’ll experience back pain. In 2015, a comprehensive review of studies looking at imaging findings in people without back pain found that disc herniation was present in 29 percent of individuals 20-29 years old. That increased to 43 percent for those who were 80-89 years old.
Disc bulges were even more common, with 50 percent of individuals 40-49 years old showing imaging findings of a disc bulge without back pain.5
Can imaging lead to unnecessary surgery?
Tough question. Rather than thinking about surgery as being necessary or unnecessary, let’s review what we know about imaging and disc injuries:
- Disc injuries, bulges or herniations do not necessarily cause back pain.
- If you have back pain and imaging indicates a disc injury, your pain is not necessarily caused by the disc.
- Disc degeneration, bulges, and herniations are not unusual.
- Imaging, whether x-ray, MRI, or CT scan, is not always accurate. Over the course of the night while we sleep, we gain roughly 16 percent of the volume in our discs,6 meaning we gain roughly 1.4 percent of our overall height over the course of a night’s sleep!7 Therefore, if you have a morning appointment for an MRI, your discs may look different than if you had an evening appointment.
- Images require interpretation, and there can be significant variability between those interpreting results. A study in 2017 looking at variability in lumbar spine MRI analysis found that the average miss rate for disc herniations was 47.5 percent.8
- Discs have the capacity to heal without surgical intervention.
The last fact is perhaps the most important of all. The human body has a tremendous capacity to self-heal, and spinal discs are no exception. There is ample blood supply near the spine, and through different inflammatory and immune reactions to injury, the body will be able to repair and heal with time. While different sized herniations will take different lengths of time to heal, and there are other factors that can impact healing, scientific evidence shows that discs can heal after an injury without surgery. In fact, roughly 2/3 of people who have disc herniations will eventually have no imaging evidence they ever had a disc herniation,9and 90 percent will show greater than 50 percent reduction in size after 12 months.10

Not only do we know that disc injuries can heal without surgery, but also, people who have disc herniations and back pain will often have a significant reduction in back pain before the disc is healed. While the average time it takes to show good disc healing in imaging studies is roughly 6-12 months, the average time for back pain relief is closer to 4-8 weeks for those who have back pain at all.11,12
What does a herniated disc feel like?
While the experience of pain with a herniated disc will have some variation from person to person, commonalities between experiences include:
- Leg or buttock pain (typically on just one side).
- Difficulty with sitting (due to pain).
- Pain with bending forward (as if to touch your toes).
- Standing or laying down will commonly relieve pain.
While these four experiences are the most classic signs and symptoms of a herniated disc, additionally, some people may experience numbness and tingling in their legs, weakness, or sharp shooting pains down their leg that are intense but brief. Coughing or sneezing may make the pain worse in more aggravated situations. While a disc herniation may be present before pain, there will typically be some reason why it became painful.2,13
Disc injuries can occur due to a variety of reasons, but the most common reasons for the onset of pain that we typically see in our clinics include:
- Overloading the back with too much weight
- i.e., picking up something heavy
- Doing a repetitive activity or motion
- i.e., repeatedly bending down to pick something off the floor, or twisting while shoveling
- Excessive sitting
How can physical therapy help with a herniated disc.
While a herniated disc can occur anywhere along the spine, it most often occurs in the lower back and is one of the most common causes of low back pain. With low back pain (LBP) being a widespread, global problem that creates substantial personal and financial burdens,13,14 a lot of time, energy, and resources have been allocated toward a better understanding of how we can avoid it.
Broadly speaking, engaging in a specific and well-designed exercise program has been shown to be an effective method in preventing episodes of low back pain as well as in treating non-specific low back pain. 13,15,16,17
Physical therapy is an ideal choice for addressing all types of back pain, including back pain due to a herniated disc. As musculoskeletal experts, PTs have the education and experience to help patients overcome the pain and dysfunction related to spinal disc issues, to minimize the chance of injury and to avoid reinjury.
Pursuing physical therapy at the onset of pain can significantly lower the need for advanced imaging, spinal injections, surgery, and the use of opioids, as patients who receive physical therapy early have 60 percent lower total LBP-related costs over a two-year span compared to those who delay physical therapy.18
A customized PT plan of care – including prescribed exercises that focus on strengthening muscles to stabilize the spine – can help patients get back to the things they love, return to work and avoid surgery. If surgery is unavoidable, physical therapy is an excellent option for pre- and post-operative care.
Some people may have persistent pain from disc herniations for a variety of reasons that will ultimately cause them to seek surgery. While a larger disc herniation may have a greater chance of needing surgery, other factors can impact the ability of the disc to heal to avoid surgery, such as being an active smoker or having a Body Mass Index (BMI) greater than 30 kg/m2.
Ultimately, about 10 percent of people experiencing disc herniation will be treated surgically.21 If surgery is necessary, physical therapy can be helpful in advance of the procedure to help minimize dysfunction of the musculoskeletal system after surgery.23 Following surgery in which part of the disc is removed, called discectomies, a person’s trunk muscle strength is decreased by roughly 30 percent and thus engaging in an exercise program is critical for optimal recovery.24 Committing to an 8-week program focused on stabilization exercises for the low back under the supervision of a physical therapist can help reduce pain, improve strength and mobility, and has shown to have better post-operative results than either doing simple exercises at home or doing nothing at all.24
While disc herniation and low back pain can feel overwhelming and might be complicated, we have ample evidence that illustrates that exercise can help reduce the likelihood of a disc injury occurring, improve both non-surgical and surgical outcomes and help minimize the risk of developing chronic back pain. If you have back pain, or a concern about a possible disc injury, don’t wait! Seek the advice of your physician, physical therapist, or another qualified health provider. The sooner you address your situation, the faster and more optimal your outcome will be.
REFERENCES
- Dutton M(Ed.), (2017). Dutton’s Orthopedic Examination, Evaluation, and Intervention, 4e. McGraw Hill.
- NAIOMT C-511: Lumbopelvic I Resource Guide Version 4.0
- Goode AP, Marshall SW, Renner JB, Carey TS, Kraus VB, Irwin DE, Stürmer T, Jordan JM. Lumbar spine radiographic features and demographic, clinical, and radiographic knee, hip, and hand osteoarthritis. Arthritis Care Res (Hoboken). 2012 Oct;64(10):1536-44.
- Jarraya M, Guermazi A, Lorbergs AL, Brochin E, Kiel DP, Bouxsein ML, Cupples LA, Samelson EJ. A longitudinal study of disc height narrowing and facet joint osteoarthritis at the thoracic and lumbar spine, evaluated by computed tomography: the Framingham Study. Spine J. 2018 Nov;18(11):2065-2073. .
- Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, Halabi S, Turner JA, Avins AL, James K, Wald JT, Kallmes DF, Jarvik JG. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015 Apr;36(4):811-6.
- Botsford DJ, Esses SI, Ogilvie-Harris DJ. In vivo diurnal variation in intervertebral disc volume and morphology. Spine (Phila Pa 1976). 1994 Apr 15;19(8):935-40.
- McMillan DW, Garbutt G, Adams MA. Effect of sustained loading on the water content of intervertebral discs: implications for disc metabolism. Annals of the Rheumatic Diseases 1996;55:880-887.
- Herzog R, Elgort DR, Flanders AE, Moley PJ. Variability in diagnostic error rates of 10 MRI centers performing lumbar spine MRI examinations on the same patient within a 3-week period. Spine J. 2017 Apr;17(4):554-561.
- Zhong M, Liu JT, Jiang H, Mo W, Yu PF, Li XC, Xue RR. Incidence of Spontaneous Resorption of Lumbar Disc Herniation: A Meta-Analysis. Pain Physician. 2017 Jan-Feb;20(1):E45-E52.
- Takada E, Takahashi M, Shimada K. Natural history of lumbar disc hernia with radicular leg pain: Spontaneous MRI changes of the herniated mass and correlation with clinical outcome. J Orthop Surg (Hong Kong). 2001 Jun;9(1):1-7.
- Ahmed Rizk Elkholy, Ashraf Mohamed Farid, Ebrahim Ahmed Shamhoot, Spontaneous Resorption of Herniated Lumbar Disk: Observational Retrospective Study in 9 Patients. World Neurosurgery, Volume 124, 2019,Pages e453-e459.
- Mohamed Macki, Marta Hernandez-Hermann, Mohamad Bydon, Aaron Gokaslan, Kelly McGovern, Ali Bydon, Spontaneous regression of sequestrated lumbar disc herniations: Literature review, Clinical Neurology and Neurosurgery, Volume 120, 2014, Pages 136-141.
- Steffens D, Maher CG, Pereira LS, Stevens ML, Oliveira VC, Chapple M, Teixeira-Salmela LF, Hancock MJ. Prevention of Low Back Pain: A Systematic Review and Meta-analysis. JAMA Intern Med. 2016 Feb;176(2):199-208.
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, Woolf A, Vos T, Buchbinder R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012 Jun;64(6):2028-37.
- Bigos SJ, Holland J, Holland C, et al. High-quality controlled trials on preventing episodes of back problems: systematic literature review in working-age adults. 2009. In: Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. York (UK): Centre for Reviews and Dissemination (UK); 1995.
- Hayden JA, van Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev.2005.
- Macedo LG, Maher CG, Latimer J, McAuley JH. Motor control exercise for persistent, nonspecific low back pain: a systematic review. Phys Ther. 2009;89:9-25.
- Childs, J.D., Fritz, J.M., Wu, S.S. et al. Implications of early and guideline adherent physical therapy for low back pain on utilization and costs. BMC Health Serv Res 15, 150 (2015)
- França FJR, Callegari B, Ramos LAV, Burke TN, Magalhães MO, Comachio J, CarvalhoSilva APMC, Almeida GPL, Marques AP. Motor Control Training Compared With Transcutaneous Electrical Nerve Stimulation in Patients With Disc Herniation With Associated Radiculopathy: A Randomized Controlled Trial. Am J Phys Med Rehabil. 2019 Mar;98(3):207-214.
- Ye C, Ren J, Zhang J, Wang C, Liu Z, Li F, Sun T. Comparison of lumbar spine stabilization exercise versus general exercise in young male patients with lumbar disc herniation after 1 year of follow-up. Int J Clin Exp Med. 2015 Jun 15;8(6):9869-75.
- Bakhtiary, Amir & Safavi-Farokhi, Ziaeddin & Rezasoltani, Asghar. (2005). Lumbar stabilizing exercises improve activities of daily living in patients with lumbar disc herniation. Journal of Back and Musculoskeletal Rehabilitation. 18. 10.3233/BMR-2005-183-401.
- Zhao, Wei-Ping MD; Kawaguchi, Yoshiharu MD, PhD; Matsui, Hisao MD, PhD; Kanamori, Masahiko MD, PhD; Kimura, Tomoatsu MD, PhD. Histochemistry and Morphology of the Multifidus Muscle in Lumbar Disc Herniation, Spine: September 1, 2000 – Volume 25 – Issue 17 – p 2191-2199.
- Colakoglu, B., & Alis, D. (2019). Evaluation of lumbar multifidus muscle in patients with lumbar disc herniation: are complex quantitative MRI measurements needed?. The Journal of international medical research, 47(8), 3590–3600.
- Yílmaz F, Yílmaz A, Merdol F, Parlar D, Sahin F, Kuran B. Efficacy of dynamic lumbar stabilization exercise in lumbar microdiscectomy. J Rehabil Med. 2003 Jul;35(4):163-7.
Get Started Today
We offer comprehensive, expert treatment for a variety of neck and back problems. Your physical therapist will perform a thorough evaluation and if PT is determined to be the best course of care, will create a custom treatment plan including movement, hands-on care, and patient education.


