When pain is sticking around, those who are suffering can change their lives by working consistently on the following:
- Aerobic exercise
- Understanding how pain works
- Proper sleep practices
- Paced increases of activities to reach goals
You may be wondering why some of these four things have been found to be so important to reduce pain. And maybe you’re asking, “How do they work?”
“Your pain may be in your head.”
Most of us have heard this saying before. It’s certainly not something that anyone who is suffering wants to hear. And the reason we don’t like hearing it is because it makes us feel dismissed and as if our pain is not real.
Yet it is now widely accepted that all pain is constructed by the brain (yes, in the brain, which is in our heads) in response to what we think is threatening or dangerous to us.
Whether you step on a nail, stub your toe, or are agonized by back pain and sciatica for 10 years … pain is an experience that occurs in the brain. So, while injury and irritation do occur at other parts of the body, it is the brain that actually controls if you will experience pain or not.
For example, if you sprain your wrist, the damaged tissue signals the nerves at your wrist to send up danger messages to the brain, then the brain gives these signals some thought and produces pain to protect you. This happens in milliseconds, so you don’t really notice any delay in time from when you injure yourself to when you begin feeling pain. It is often an immediate response. So, in this case it is the injured wrist tissues that trigger the message that becomes pain, but it is the brain itself that is responsible for the experience of that pain.

Does a physical therapist only help pain that is the result of injury?
What about persistent or chronic pain? We know that pain is not just the result of tissue damage or injury, because 20 percent of the population continues to suffer from some form of ongoing pain after injured tissues have had time to heal.
Physical therapists are experts at performing skilled examinations to discover the presence and extent of injury. When a person in pain sees a PT at Therapeutic Associates, they can expect a thorough first visit where they share the story of their pain, then have the PT perform many gentle tests to find out more about what’s contributing to their problem. A plan for treatment is discussed, which may involve learning what’s needed to help an injury heal and recover, which should resolve the pain. A shift in thinking is quickly made when tissues are found to be un-injured, but pain continues to stick around. In these cases, treatment is directed at the pain itself, not at helping to heal an actual injury.
We now understand that many treatments in physical therapy work to reduce pain, but should be paired with a talk about what pain actually is. When a PT takes the time to “explain pain” to a patient, that patient experiences less pain! Also, explaining pain to people has been shown to reduce disability and improve function.
Why does explaining pain work?
The brain has the amazing ability to release “pain killing” chemicals that are strong enough to stop a danger signal coming in from the tissues of the body. This can change, or even eliminate the pain experience. If we’re suffering with pain and we understand how these signals work and how the brain is a large part of things, then we are often able to “tap in” to the release of these pain killing chemicals!
Below is an actual brain scan of a person with ongoing pain that has been given different explanations in the past for her pain. Treatments for the pain have not helped.
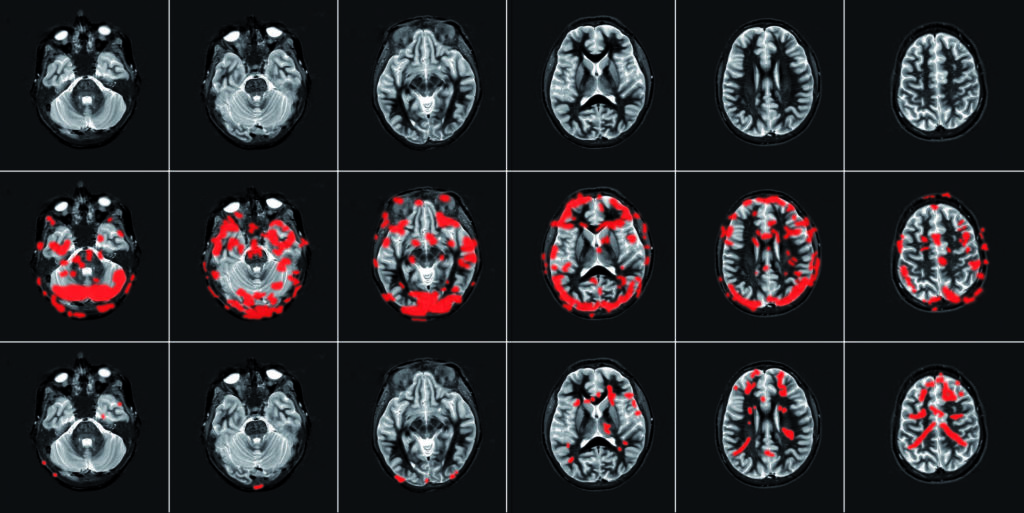
- Row 1: The person is relaxing in the scanner, and you can see the brain is calm — no red blobs.
- Row 2: The person moves her painful back. Many red blobs show us that her brain is working through the danger signals it’s received. She’s in pain!
- Row 3: The same person attends a short session where a physical therapist explains how pain works (how the nerves and brain become more sensitive to protect the painful area and how this can go on and on, even after an injury has healed. How the pain does not mean that any damage is actually happening and that her tissues do not have to be injured for her to feel pain). Then she repeats the same back movement that caused the pain in Row 2. This time there are fewer red blobs on the scan, showing us that her pain has decreased.
So … is that all PT can do to treat pain? Is learning about pain enough?
The answer, not surprisingly, is no. Talking about how pain works needs to happen along with other “typical” treatments most of the time (manual therapy, exercise, pacing of activities, mindfulness/meditation, etc.). And everyone needs to take an active role in their own treatment.
Connection and trust between a person and their physical therapist is key. Patients need to be engaged, be actively involved in the planning of their care and feel empowered during treatment. Part of this approach to patient-centered care, known as shared decision making, is helping patients learn to “own” their pain and to be responsible for working on it both through their partnership with their PT and independently.

Oh, and one more thing — don’t forget that one of the quickest, easiest ways to decrease pain is to move. “Motion is lotion” is a favorite PT saying and it’s true! When we move, we increase blood circulation to tissues, create space and ease pressure on our body and increase our natural joint lubricant to our joints. PTs are experts in movement and can help you understand how important it is to keep moving to avoid pain.
We look forward to being a part of your healthcare team.
From injury recovery to understanding and managing pain, patient success is our passion. Our therapists are committed to patient education and to the application of evidence-based treatment techniques to ensure you experience the best in rehabilitation and preventative care.


